Reverse Shoulder Replacement
A reverse shoulder replacement can be life changing - reducing constant pain, restoring mobility, and bringing back independence. With careful surgical planning, advanced technology, and structured rehabilitation, the vast majority of patients experience dramatic and lasting improvements in their quality of life.
What is a Reverse Shoulder Replacement?
Your shoulder is a ball and socket joint. In some people, a combination of genetics, age, previous trauma and rotator cuff tears can lead to the shoulder “wearing out”. This means that the cartilage which normally allows the shoulder to move and glide freely wears away, leaving a bone on bone ball and socket joint – or arthritis.
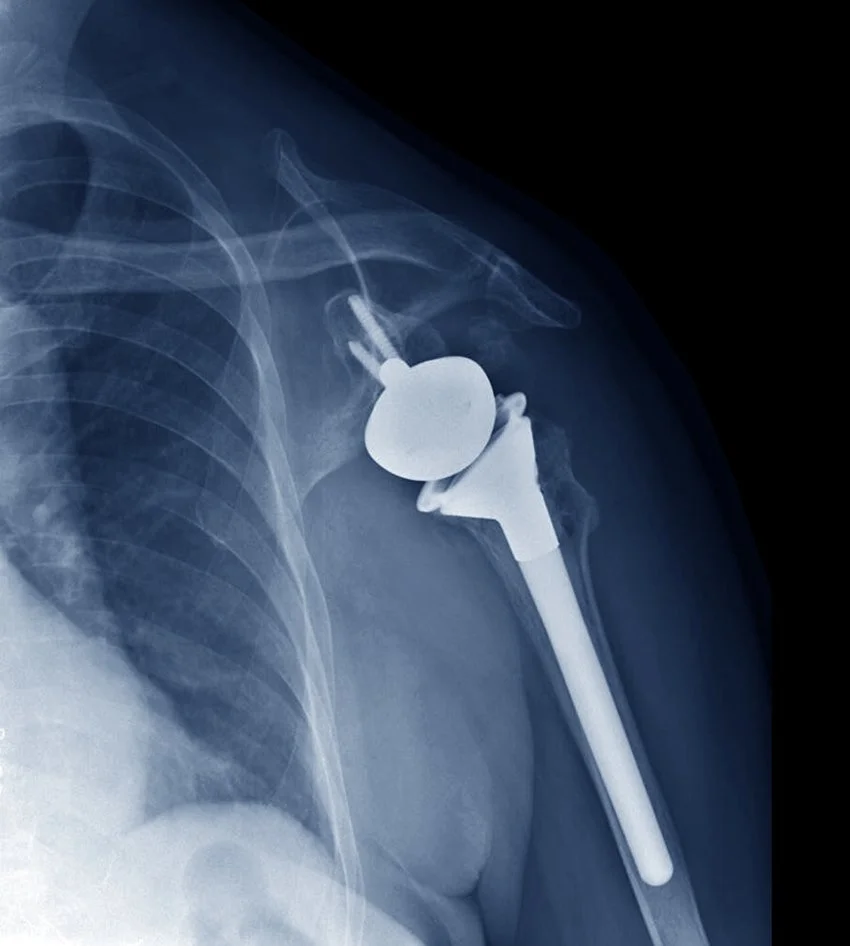
A reverse total shoulder replacement involves removing the worn out ball (humerus) and socket (glenoid) from your shoulder, and replacing them with metallic and plastic components. To help recruit other muscles around the shoulder and give better range of motion and function, we switch the orientation of the ball and socket, so now the ball is on the glenoid side, and the socket is on the humeral side.
Who Should Consider Reverse Shoulder Replacement?
You may be a candidate for reverse shoulder replacement if you have:
Persistent, debilitating shoulder pain affecting sleep and daily life
Difficulty with overhead activities
Stiffness or loss of shoulder motion that limits activity
Pain not relieved by nonsurgical treatments (medications, injections, physiotherapy)
The most common reason is advanced osteoarthritis, but other causes include rheumatoid arthritis, avascular necrosis (poor blood supply leading to bone collapse), rotator cuff arthropathy, and posttraumatic arthritis after an injury.
How is Reverse Shoulder Replacement Performed?
Mr. Kirzner performs reverse shoulder replacement surgery through an anterior deltopectoral approach. It’s done through a ~10cm incision down the front of the shoulder and takes approximately 60- 120 minutes to perform.
You will be asleep for the duration of the operation (ie a general anaesthetic). The anaesthetist will talk to you about a nerve block before the operation, which helps with pain relief and generally lasts 24-48 hours. This is normally done while you are sedated/half asleep just prior to the operation.
The steps involved in reverse shoulder replacement surgery include:
Approach:
10cm incision down front of arm
Internervous plane between deltoid and pectoral muscles is formed
Subscapularis muscle reflected off humerus and capsulotomy performed
Bone preparation:
The damaged humeral head (ball) and the worn-out glenoid (socket) are removed
The glenoid is prepared using reamers (large cheese graters) and the humerus using broaches to ensure proper sizing and fit of the components.
Advanced preoperative planning and Patient Specific Instrumentation (PSI) may be used in order to increase the accuracy of bone preparation and improve the implant positioning
Implantation:
Artificial implants made of cobalt chromium and titanium alloys are positioned to recreate the joint surfaces and restore alignment and function.
The humeral stem will be inserted into the humerus and the new glenoid will be inserted with a central peg and screws to secure it. These can be either uncemented or cemented depending on your bone quality.
A glenosphere (ball) is attached to the socket and the humeral component is lined with a plastic to form your new joint
Steps are taken to achieve correct length, mobility, and joint stability as this ensures stable function and longevity of the shoulder implant.
Your Recovery & Follow-Up Schedule
2 Weeks: The wound is kept clean and dry. At your review, dressings are removed and healing is checked. Dissolvable sutures mean no stitches need removing.
6 Weeks: Patients are usually off all strong pain relief medication, and back to driving and light work. For the first 6 weeks avoid putting your arm behind your back – like tucking in a shirt or toileting. Avoid pushing up from a chair. When getting changed, put your operated arm in the sleeve first. No heavy lifting.
3 Months: A repeat clinical check and Xray is performed. For the first 12 weeks avoid pushing down on your operated arm (eg pushing up out of a chair)
12 Months: Most patients will achieve a pain-free shoulder with a functional range of motion. You should be able to freely reach key areas like the top of your head and toileting behind your back. Xrays are performed to confirm stable implant fixation.
Longterm: If all progresses as expected, follow-up Xrays and assessments are performed at 5year intervals to monitor implant health.
Learn More About Reverse Shoulder Replacement Surgery:
What are the risks of Reverse Shoulder Replacement Surgery?
Reverse shoulder replacement surgery is generally safe but, like any major procedure, it carries risks. These include:
Infection: Usually only a superficial wound infection to the top-most layer of the skin. In rarer cases a deep infection can develop and this is a serious complication that may require further surgery and exchange of the implants. Rare but serious, <1%.
Stiffness and ongoing pain: 1-20 in every 100 people will have some mild ongoing pain or stiffness in the shoulder after the operation
Damage to the nerves and blood vessels around the shoulder: Rare but serious, <1%
Clots – Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE): These are very rare in upper limb surgery, and much lower when compared to lower limb cases like hip and knee replacements. Rare and affects <1%
Shoulder Dislocation: This is very uncommon and could suggest another complication like infection. Occurs between 1-5 cases per 100
Loosening of the Implants: This is not likely to happen for many years after the surgery. The implants used by Mr Kirzner have an excellent track record in the AOA National Joint Registry
We will go through your personal risk profile and ensure that every step is taken to minimise complications and maximise success. The fitter and stronger you are prior to your surgery, the safer and quicker your recovery will be and the more you will get out of your shoulder.
What does the recovery look like?
You will wake up with your arm in a sling after your surgery. If you have had a nerve block, you shouldn’t feel any pain till the next day. The nurses will provide you pain relief and the next morning a physio will see you to go through some exercises you can do to help strengthen the muscles around the shoulder and stop the shoulder from becoming too stiff.
These exercises will change over the next few months but you should try to do them regularly to maximise your rehabilitation. Early rehabilitation focuses on regaining walking ability and strength.
Most patients spend 1-2 days in hospital after surgery, before going home. A number of allied health staff (physios, occupational therapists) will make sure you have adequate support at home before discharge. An appointment will be made for you for a wound check
Will it Set Off the Metal Detector at an Airport?
Yes, it's possible that the metal components in a shoulder replacement will set off airport metal detectors. Be proactive and advise the security guards that you have had a shoulder replacement. Having a letter or medical certificate will not prevent these security measures.
When Can I Drive After a Reverse Shoulder Replacement?
To drive you will need to be off all strong pain relief and out of your sling and have the ability to perform an emergency stop safely. For most patients this takes 6 weeks.
When Can I Fly After a Reverse Shoulder Replacement?
Short flights are often safe within a few weeks after surgery, but longer flights may increase the risk of blood clots. This is less of an issue compared with lower limb joint replacement surgery.
What about sports and hobbies after a Reverse Shoulder Replacement?
Gentle swimming (breastroke not freestyle): after 12 weeks
Gardening (light tasks only): 8-12 weeks
Bowls: after 3-6 months
Golf, tennis, badminton, squash: after 4-6 months
Do I Need Antibiotics After a Reverse Shoulder Replacement for Dental Work?
For the first 3 months following a shoulder replacement you should be given antibiotics by your dentist if you require urgent dental work. This is to prevent bacteria from your mouth entering your bloodstream and travelling to the shoulder joint.
After 3 months routine antibiotics are not required for dental work unless your immune system is compromised. If you are in doubt, please get your dentist to contact us prior to your dental procedure.
Is the surgery painful?
We use a multimodal pain control approach, including local anaesthetic, nerve blocks, and tailored medication. Pain is usually well managed, and many patients describe it as far less painful than they expected. Most patients are discharged on medications no stronger than paracetamol and ibuprofen.