Partial Knee Replacement
Partial knee replacement is a modern, minimally invasive treatment for arthritis limited to one compartment of the knee. It provides excellent pain relief, a quicker recovery, and a more natural-feeling knee for the right patients.
With careful selection, precision surgery, and structured rehabilitation, outcomes are consistently excellent and long-lasting.
What is a partial knee replacement surgery?
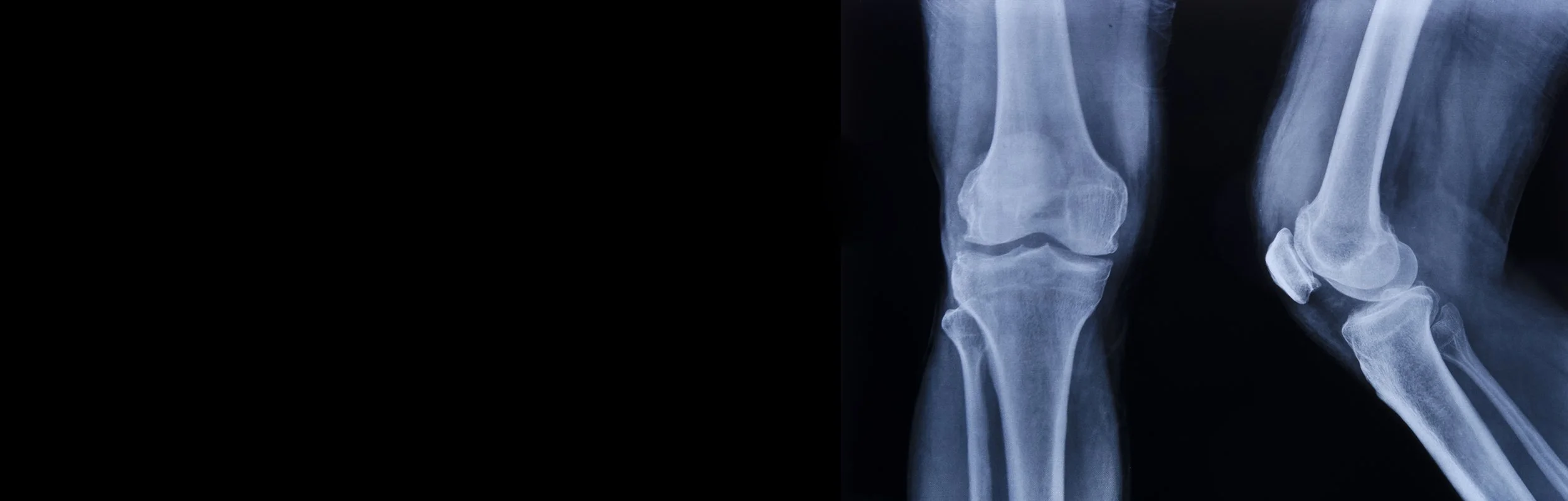
A partial knee replacement, also called a unicompartmental knee replacement, is a surgical procedure in which only the damaged part of the knee joint is replaced, while the healthy bone, cartilage, and supporting ligaments are preserved.
Your knee is made up of three compartments:
Medial compartment – the inside of the knee (closest to the other leg)
Lateral compartment – the outside of the knee
Patellofemoral compartment – underneath the kneecap and the groove it slides in
In around half of patients with knee arthritis, only one of these compartments is affected. In such cases, a partial knee replacement can be an excellent option.
This surgery offers several advantages over a total knee replacement:
Smaller incision and less invasive operation
Faster recovery and rehabilitation
Preservation of normal knee motion
A knee that feels more "natural," as the healthy compartments and ligaments (including the anterior cruciate ligament – ACL) are left intact
Lower blood loss and fewer complications in appropriate patients
Robotic-assisted surgery can further improve the precision of implant positioning, tailoring the procedure specifically to your unique knee anatomy.
Who is suitable for a Partial Knee Replacement?
A partial knee replacement may be right for you if:
Your arthritis is limited to one compartment of the knee
You have ongoing pain and stiffness not relieved by physiotherapy, medications, or injections
You have a preserved range of motion and stable ligaments
Deformity of the knee (bow-leg or knock-knee) is mild and correctable
It may not be suitable if you have:
Arthritis affecting multiple compartments
Severe stiffness or loss of motion
Significant ligament damage (especially ACL deficiency)
Severe deformity that cannot be corrected
In such cases, a total knee replacement may be a more appropriate option.
What is involved in partial knee replacement surgery?
The steps involved in knee replacement surgery include:
Approach:
A smaller, targeted incision is made on the front of the knee, compared to total knee replacement.
The kneecap is moved to one side to allow access to the affected compartment.
Bone preparation:
The worn cartilage and thin layers of bone from the affected compartment are removed.
Importantly, the cruciate ligaments are preserved, along with the unaffected compartments.
Robotic assistance may be used to enhance accuracy and tailor the implant to your knee.
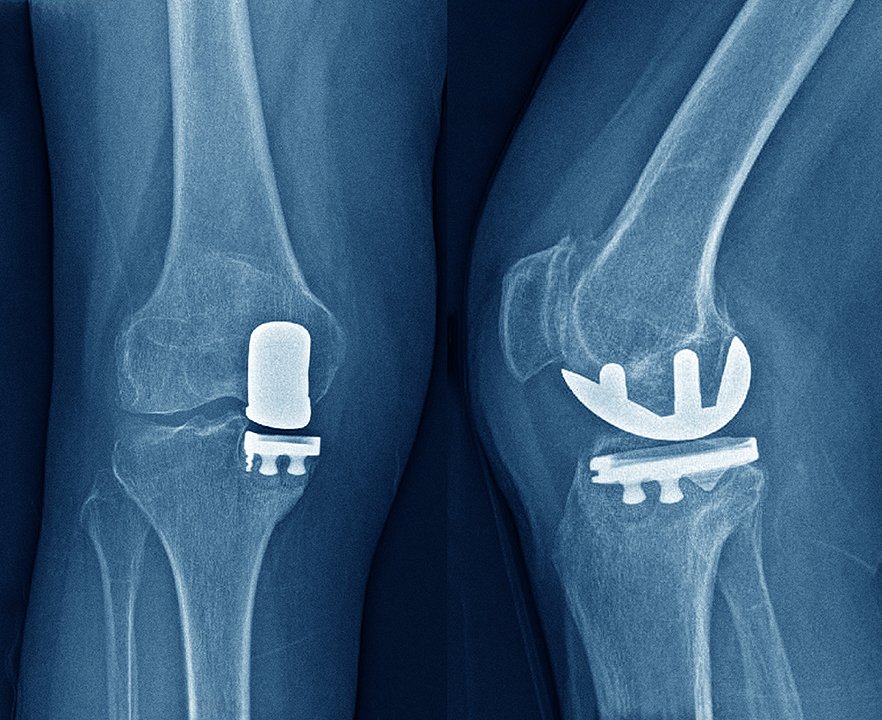
Implantation:
Highly durable cobalt-chromium or titanium implants are cemented into place.
A smooth polyethylene (medical-grade plastic) spacer is inserted between the metal pieces, allowing natural, gliding movement.
Alignment and balancing:
The surgeon checks knee motion, stability, and balance, making minor adjustments to achieve optimal function before closing the wound.
Your Recovery & Follow-Up Schedule
Because a partial knee replacement is less invasive, recovery is usually quicker than with a total knee replacement.
2 weeks: The wound is checked, and dressings are removed. Most patients are walking without crutches and have returned to light activities.
6 weeks: Most patients can straighten the knee fully and bend it beyond 90 degrees. Strong painkillers are rarely required, and many patients have returned to driving and work.
3 months: An X-ray from hip to ankle is performed to confirm alignment. Day-to-day activities are usually much easier, with improved mobility and walking distance.
12 months: Most patients enjoy a pain-free knee with a near-normal feel and function. Another X-ray checks implant stability.
Long term: Follow-up X-rays are recommended every 5 years to ensure the implant and other compartments remain healthy.
Frequently Asked Questions
What are the risks of Knee Replacement Surgery?
Knee replacement surgery is generally safe but, like any major procedure, it carries risks. These include:
Blood clots: in the leg veins, which can travel to the lungs (pulmonary embolism). This risk can be reduced by early movement, blood thinners, and compression devices.
Infection: which is minimized by sterile surgical techniques and antibiotics. If you are concerned about an infection, please call the rooms and do not start antibiotics until speaking with Mr. Kirzner
Postoperative pain and stiffness: this can often be managed with medication and physiotherapy. Occasionally this may require further surgery for manipulation or arthroscopic release
Implant problems: loosening, wear, or rarely, mechanical failure may occur over time, sometimes requiring revision surgery.
Nerve or blood vessel injury: though this is uncommon, nerve or blood vessels around the knee can be injured during surgery.
Dissatisfaction or ongoing pain: Previous studies quote a 10-20% rate of dissatisfaction with total knee replacement surgery. Thankfully with appropriate indications, patient selection, expectation setting and modern technologies and techniques, satisfaction rates have improved.
Patients younger than 55 have the least satisfaction after knee replacement, higher expectations and demands is a big element of this.
Numbness and difficulty kneeling: the incision for knee replacement surgery can damage the small nerves around the front of your knee causing numbness on the outside/lateral aspect of your scar. Some patients report difficulty kneeling, however this can be worked on with exercises to desensitise and use of padding to assist. If you regularly kneel for work or recreation, a lateral incision can be performed to decrease this issue.
Progression of disease: Sometimes, arthritis will progress to involve other compartments in the knee, and patients may develop pain from arthritis in a different location. This will require a revision to a total knee replacement, which is technically straightforward and has a high success rate.
We will go through your personal risk profile and ensure that every step is taken to minimise complications and maximise success. The fitter and stronger you are prior to your surgery, the safer and quicker your recovery will be and the more you will get out of your knee.
Outcomes of a partial knee replacement?
The benefits of this surgery include quicker recovery, preservation of knee motion, and a more "natural" feeling compared to total knee replacement. Studies along with the Australian Joint Registry, show excellent long-term function, although revision rates are slightly higher than total replacements (10–15% at 10 years).
The key advantage is that most patients report very high satisfaction, lower rates of dissatisfaction compared with total knee replacement, and excellent function. If arthritis progresses, conversion to a total knee replacement is usually smooth and effective.
Will it Set Off the Metal Detector at an Airport?
Yes, it's possible that the metal components in a knee replacement will set off airport metal detectors. Be proactive and advise the security guards that you have had a knee replacement. Wear clothing where the knee incision can easily be shown to the security staff. Having a letter or medical certificate will not prevent these security measures.
Will My Knee Look Different After the Replacement?
Depending on your level or arthritis and deformity, your knee may appear straighter than before and also may be 3-4mm longer. With time the majority of patients adjust to any difference.
When Can I Drive After a Knee Replacement?
To drive you will need to be off all strong pain relief and crutches and have the ability to perform an emergency stop safely. For most patients this is 3 weeks for a left knee (automatic car) and 4-6 weeks for a right knee.
When Can I Fly After a Knee Replacement?
Short flights are often safe within a few weeks after surgery, but longer flights may increase the risk of blood clots. In general, precautions like compression stockings and in-seat exercises are recommended for several weeks.
When Can I Swim After a Knee Replacement?
Participating in pool-based rehabilitation or swimming is not recommended for 4 weeks after your operation as it may increase the risk of infection.
Do I Need Antibiotics After a Knee Replacement for Dental Work?
For the first 3 months following a knee replacement you should be given antibiotics by your dentist if you require urgent dental work. This is to prevent bacteria from your mouth entering your bloodstream and travelling to the knee joint.
After 3 months routine antibiotics are not required for dental work unless your immune system is compromised. If you are in doubt, please get your dentist to contact us prior to your dental procedure.
Will I be able to return to sport?
Most patients return to low-impact activities like walking, cycling, golf, swimming, and hiking. Running and other high-impact sports are not recommended due to wear risk.
Is the surgery painful?
We use a multimodal pain control approach, including local anaesthetic, nerve blocks, and tailored medication. Pain is usually well managed, and many patients describe it as far less painful than they expected. Most patients are discharged on medications no stronger than paracetamol and ibuprofen.