Revision Knee Replacement
Revision knee replacement is a complex but highly effective procedure designed to give patients a second chance at a stable, pain-free knee when their initial replacement develops problems.
With modern implants, robotic planning tools, and detailed recovery programs, outcomes continue to improve, helping patients return to a more comfortable, active, and functional lifestyle.
What is a revision knee replacement?
A revision knee replacement involves removing part or all the old knee implants which have failed or worn out and inserting new prosthetic components. This procedure is often more complex than a primary knee replacement, as it may involve dealing with bone loss, scar tissue, or infection, and sometimes additional procedures like bone grafting. The surgery aims to relieve pain, correct alignment and leg length, rebuild bone where needed, and restore a reliable, stable knee for everyday life.
Indications for Revision Knee Replacement
Revision surgery is generally recommended for the following reasons:
Implant wear or loosening
Infection of the prosthetic joint
Instability or recurrent dislocation of the knee
Persistent pain or stiffness
Fracture near the prosthesis
Osteolysis (bone loss around the implant)
Mechanical failure of the implant or its components
Preoperative Workup
Revision surgery requires careful planning and investigation to identify the cause of implant failure and prepare for the best possible outcome. The workup usually includes:
Clinical assessment: Discussion of your symptoms (pain, instability, swelling, deformity) and functional limitations
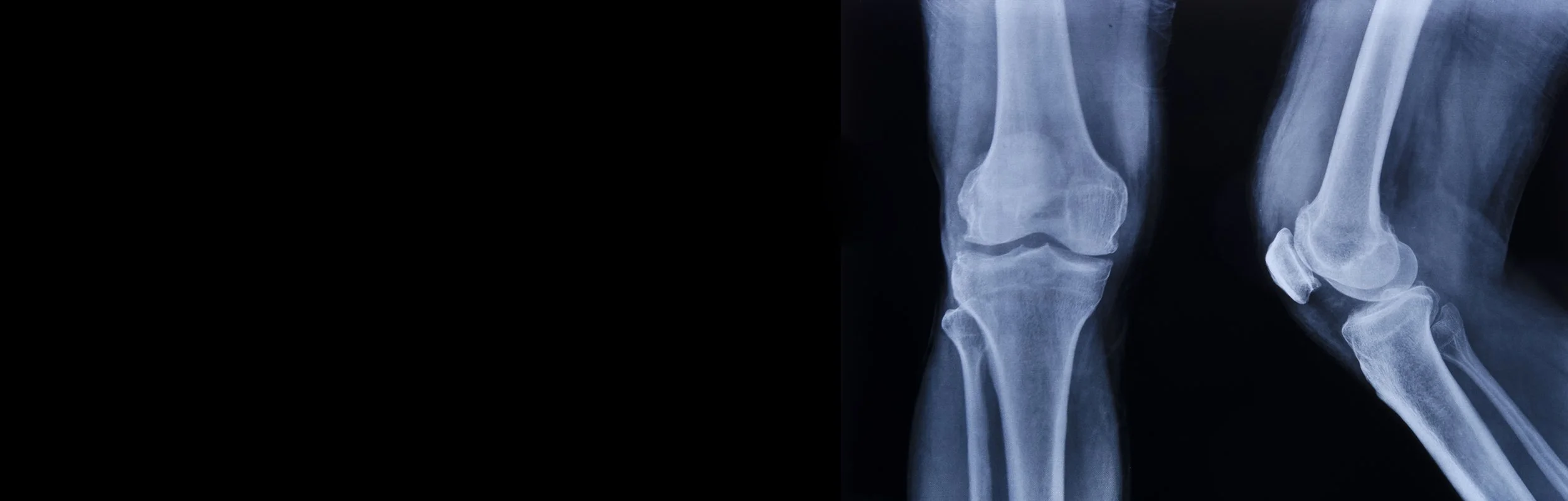
Imaging: X-rays, CT scans, MRI or sometimes CT SPECT scans to evaluate implant position, fixation, and bone quality
Blood tests: Checking for signs of low-grade infection or inflammation
Joint aspiration: Fluid sampling if infection is suspected
Medical history review: Including details of your prior surgery, implant type, medical conditions, and anaesthesia risks
This detailed preparation ensures the revision operation is appropriately indicated and performed safely.
What happens during Revision Surgery?
1. Surgical approach
The surgery is usually performed through the existing incision or scar from your previous replacement.
2. Removal of old components
The loose, worn, or infected implants are carefully removed.
Any old cement used to secure the original components is cleared away.
3. Reconstruction of bone and soft tissues
If there is bone loss, metal wedges, stems, sleeves, or bone grafts may be used to rebuild stability.
Ligaments and soft tissues are carefully balanced to restore knee alignment and function.
4. Insertion of new components
Specialised revision implants are used. These are built to be more robust, often longer or larger, and sometimes anchored deeper into the bone.
If infection was present, a temporary antibiotic spacer may be used before the final revision implant is inserted.
5. Closure and recovery
Surgical drains may be used to reduce swelling.
The incision is closed, and you begin rehabilitation guided by physiotherapists.
Recovery from revision knee replacement tends to be slower than with primary knee replacement due to the increased complexity of the procedure, but most patients experience improved pain relief and mobility with successful surgery.
Special Case: Two-Stage Revision for Infection
A two-stage revision knee replacement is performed when an artificial knee joint becomes infected or severely damaged. It is considered the gold standard for managing chronic periprosthetic joint infections, as it offers the best chance to eliminate infection before replacing the failed implant.
First Stage: Removal and Infection Control
The infected prosthesis is surgically removed along with any inflamed or infected tissue (aggressive debridement).
The joint is thoroughly irrigated and cleaned to eliminate bacteria and necrotic tissue.
An antibiotic-impregnated spacer is placed in the joint to maintain alignment and deliver high local concentrations of antibiotics.
Systemic antibiotics are administered, typically for 6-8 weeks, tailored to the specific organism identified during surgery.
Interim Period
The patient receives continued medical treatment and monitoring to ensure complete infection clearance, often confirmed by blood tests, imaging, and possible re-aspiration.
Second Stage: Re-Implantation
Once infection has resolved, demonstrated by negative tests and healthy wound healing, the temporary spacer is removed.
The knee joint is reconstructed with new prosthetic components, designed for stability and function, sometimes requiring additional augmentation or bone grafting if there has been bone loss.
The wound is closed, and the patient begins rehabilitation to regain strength and mobility.
Two-stage revision provides high infection cure rates but requires careful planning and a multidisciplinary approach due to its complexity and prolonged treatment period.
Your Recovery & Follow-Up Schedule
Because revision knee replacements are more complex than primary knee replacements, recovery can take longer. However, with structured rehabilitation, most patients regain excellent function.
Typical follow-up schedule:
· 2 weeks: Wound check and dressing removal. Biopsy results from the surgery are reviewed.
· 6 weeks: Clinical review and X-rays. Most patients can bend beyond 90 degrees and walk more comfortably.
· 3 months: A full-leg X-ray (hip to ankle) checks alignment. Patients are often back to most routine activities.
· 12 months: Pain relief and function are usually much improved. An X-ray checks for implant stability.
· Long-term: Ongoing review every 5 years with X-rays to assess stability.
Frequently Asked Questions
What are the risks of revision knee replacement surgery?
Revision knee replacement carries a slightly higher risk profile than first time surgery:
Infection – more common (1 in 100) than in primary total knee replacements (1 in 400), particularly in cases of previous infection. If superficial, may just require a short course of antibiotics. If deep, depending on the acuity it may require a washout and change of plastic component or exchange of all the components and an antibiotics impregnated spacer followed by another revision knee replacement once the infection is cured.
Stiffness and persistent pain – higher risk due to previously surgical scarring. This usually resolves with physiotherapy but can sometimes persist. If the knee is not bending or straightening adequately 6-8 weeks post-operatively, a manipulation procedure may be required. This involves putting the patient to sleep and pushing on the knee to break the scar tissue.
Blood Loss– may be more likely in complex reconstructions, managed with a blood transfusion if required
Nerve or vessel injury – still rare, but more likely due to scarring from previous surgery
Instability or dislocation – minimised with careful preoperative planning
Fracture – possible during removal of previous components or insertion of revision components
Implant wear or loosening over time – less common with modern revision systems
We take every precaution to reduce these risks and provide long-term success.
Outcomes: How Successful Is It?
Outcomes from revision knee replacement vary depending on the reason for revision, the patient’s health, and the complexity of the reconstruction. Most patients experience:
Significant pain relief
Improved walking stability
Restoration of function for daily life
While results are not always identical to a primary replacement, many patients achieve excellent long-term outcomes and regain independence. Studies show revision implants, especially with modern designs, last well over a decade in most patients.