Patella Stabilisation
Patella stabilisation surgery is highly effective in the right patients, restoring knee stability, preventing recurrent dislocations, and protecting your joint cartilage for the long term. The exact combination of procedures is individualised for each patient based on anatomy, activity goals, and cause of instability. With modern techniques and tailored rehabilitation, most patients return to sport and daily life with confidence and stability.
What is Patella Instability?
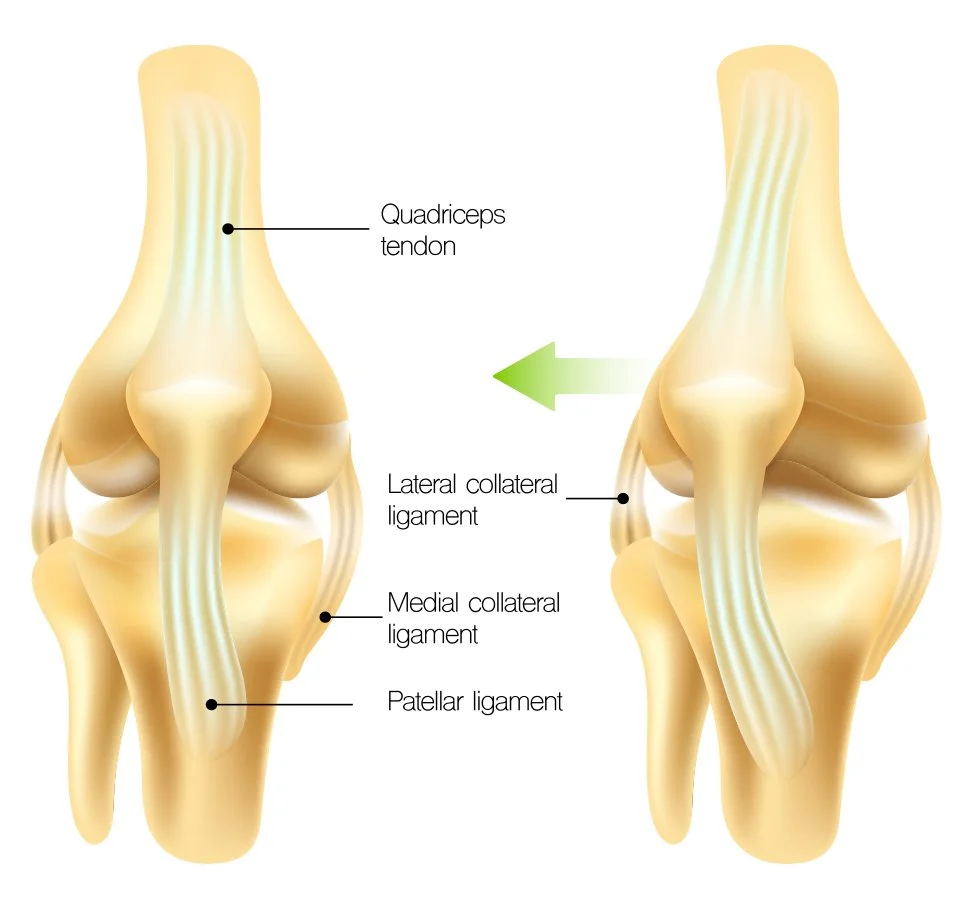
The patella (kneecap) normally sits within a groove at the end of the femur (the trochlea) and glides smoothly when you bend and straighten your knee. Certain factors—such as trauma, ligament injury, or anatomical variations—can cause the patella to slip out of place (dislocate) or feel unstable, particularly during twisting, kneeling, or pivoting activities.
A first-time dislocation is often managed without surgery. However, some patients develop ongoing instability (recurrent dislocations or the feeling that the knee will “give way”). Frequent instability episodes can cause ongoing pain, swelling, and even damage to the cartilage, increasing the risk of arthritis in the long term.
When non-operative treatments like physiotherapy, bracing, and taping are unsuccessful, patella stabilisation surgery may be recommended to restore a stable, well-aligned kneecap and protect the knee joint for the future.
Who needs Patella Stabilisation?
Surgery may be advised if you have:
Recurrent patella dislocations despite physiotherapy and non-operative care
Patellofemoral instability (kneecap repeatedly “giving way” during daily activities or sport)
Structural problems that predispose to dislocations, including absent or weak MPFL (medial patellofemoral ligament), high-riding patella (patella alta), malalignment, or shallow groove of the femur (trochlear dysplasia)
Ongoing pain, swelling, or reduced function despite conservative care
If it is your first dislocation:
80% of patients will recover without surgery if given proper rehabilitation
Surgery may still be required if there is cartilage damage with a loose body, or if your knee anatomy makes further dislocations highly likely
What Patella Stabilisation surgery involves
Surgery is tailored to your individual anatomy and the cause of your patella instability. Often, more than one technique may be required for the best result.
1. Arthroscopy (Keyhole Camera Check)
Usually performed first to inspect the joint, confirm mechanics of the patella, and treat any cartilage damage or loose fragments.
2. Medial Patellofemoral Ligament (MPFL) Reconstruction
The MPFL is the main soft-tissue stabiliser preventing the kneecap from slipping sideways.
If torn or stretched, it can be reconstructed using a tendon graft, typically taken from the hamstring.
Bone tunnels are drilled in the patella and femur, and the graft is fixed with screws or anchors.
X-rays are used during surgery to ensure correct graft placement.
This is the most common procedure performed for recurrent patella dislocations.
3. Tibial Tubercle Osteotomy (TTT)
In cases where the patella is positioned too high (patella alta) or pulled to the outside, the tibial tubercle (the bony bump where the patellar tendon attaches below the knee) is re-positioned.
It is moved downwards and/or inwards, restoring proper tracking through the femoral groove.
The bone is fixed with screws or a low-profile plate until healed.
4. Trochleoplasty (for Severe Trochlear Dysplasia)
Rarely required, but considered if the groove in the femur is very shallow or misshapen.
Trochleoplasty reshapes and deepens the trochlea groove, allowing the patella to move in a contained, stable path.
Follow-Up and Recovery Timeline
2 weeks: The knee is protected in a brace, and the wound is kept clean and dry. At your twoweek review, the dressings are removed and the brace is adjusted to allow gentle bending. Walking with crutches is common, but light weight can usually be placed through the leg.
6 weeks: Most patients will be walking independently without crutches. The knee should fully straighten and bend past 90 degrees. If an osteotomy was performed, an Xray is taken to check bone healing. Physiotherapy focuses on strength and stability.
3 months: By this stage movement and strength should feel much improved. Most people can manage daily activities with confidence. Lowimpact sport and more demanding exercises are gradually reintroduced between four to six months, guided by progress and physiotherapy.
Recovery Timeline Comparison
Patella Stabilisation
First 2 Weeks: Brace on, wound care; gentle knee bending allowed; walking with crutches, partial weight.
6 Weeks: Walking independently; knee bends >90°; X-ray if osteotomy.
3 Months: Stronger knee, normal daily activities; sport-specific rehab begins 4–6 months.
4–6 Months: Low-impact to non-contact sports, depending on progress.
9–12 Months: Full return to contact or competitive sport (if milestones achieved)
ACL Reconstruction
First 2 Weeks: Wound check; walking with crutches; focus on regaining extension.
6 Weeks: Usually walking normally, good range of motion; ongoing rehab
3 Months: Straight-line running, beginning agility drills
4–6 Months: Cutting, pivoting drills; some non-contact sport by 6 months
9–12 Months: Full contact/pivoting sport usually cleared around 9–12 months
Meniscus Surgery (Debridement / Repair)
First 2 Weeks: Debridement: Walking within days; full weight. Repair: Crutches, often partial or non-weight bearing 2–4 weeks
6 Weeks: Debridement: Near full recovery.
Repair: Still protected rehab, gradual strengthening
3 Months: Debridement: Full activity by 6–8 weeks;
Repair: Running begins 3–4 months
4–6 Months: Repair: Non-contact sport 4–6 months
9–12 Months: Repair: Return to pivoting sports at 6–9 months (sometimes up to 12)
Key Takeaways for Patients
Patella stabilisation recovery is often quicker than ACL surgery, but still requires 4–6 months of structured rehab before most sports.
ACL reconstruction has the longest return timeline, as graft healing and retraining are critical to avoid retear.
Meniscus surgery varies widely: simple debridement recovers quickly, while repairs and root repairs require slower, more protective rehab for long-term knee health.
Frequently Asked Questions
What are the risks of patella stabilisation surgery?
As with most orthopaedic procedures, infection, bleeding and blood clots are risks. Other potential specific risks of patella stabilisation surgery include:
Stiffness or loss of motion
MPFL graft failure or re-rupture with subsequent patella dislocation
Patella fracture from drilling bone tunnels
Development of osteoarthritis is a risk with ongoing patellofemoral instability
Incision site numbness
Very low risk of nerve or vessel injury
What if it’s my first-time dislocating?
Most patients dislocating for the first time can be managed with physiotherapy and strengthening of the thigh muscles. 80% of patients won’t have another dislocation with appropriate non-operative care. Some patients will have cartilage damage causing a loose body in the knee and require surgery even after only one dislocation.
What are the risk factors for ongoing instability?
Some people are more likely to experience repeated dislocations even after successful initial treatment. These include:
Ligament hyperlaxity (looser than normal ligaments)
High-riding patella (patella alta)
Shallow or flat trochlear groove (trochlear dysplasia)
Abnormal lower limb alignment or rotation
Surgical planning takes these factors into account to reduce the risk of recurrence.
When can I return to Sport?
Most patients return to sport between 3–6 months post-surgery, depending on the procedure performed and healing progress.
Physiotherapy focuses first on restoring motion, then strength, before progressing to controlled agility, running, and cutting drills.
A safe return is guided by meeting specific rehabilitation milestones, ensuring full stability before pivoting or contact sports.
Return to Sport Progression
After patella stabilisation surgery, return to sport is gradual and based on healing, strength, and physiotherapy milestones rather than a fixed calendar date. Most patients can expect the following pathway:
Gym and basic exercise (6–10 weeks): Stationary bike, pool work, and light resistance training begin once strength and range of motion improve.
Jogging and controlled drills (3–4 months): Straight-line running and lowimpact agility introduced under physiotherapy guidance.
Non-contact sports (4–5 months): Sports involving cutting and pivoting movements are added in a controlled environment.
Full contact and competitive sport (5–6 months+): Return to full activity once stability, strength, and control match the nonoperated side, with clearance from surgeon and physiotherapist.