Meniscal Surgery
What is the Meniscus?
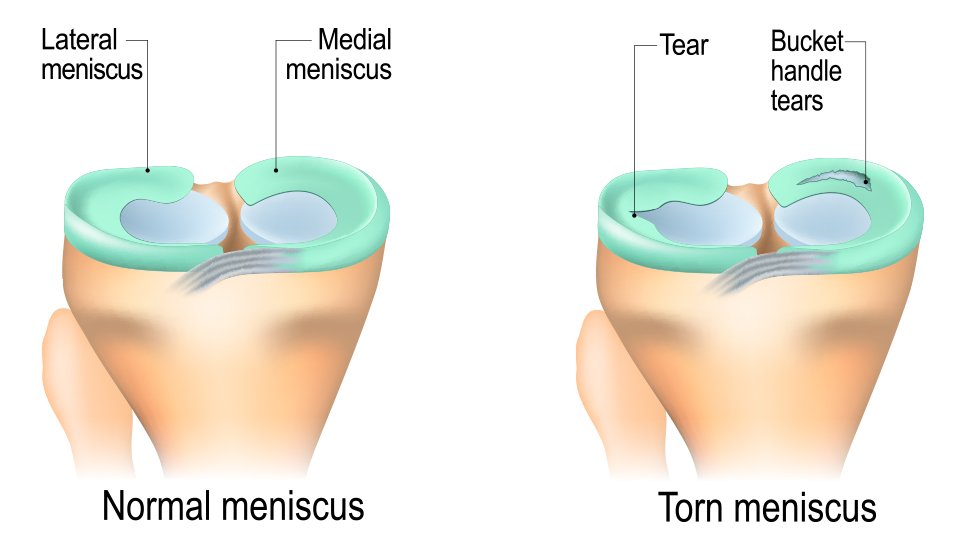
The meniscus is a C-shaped piece of fibrocartilage in the knee that acts as a shock absorber, stabiliser, and load distributor. Each knee has two menisci:
Medial meniscus – on the inner side of the knee
Lateral meniscus – on the outer side of the knee
Healthy menisci are critical for protecting the cartilage-covered bone surfaces of the knee. A torn meniscus loses its ability to cushion the joint, which can increase the risk of developing osteoarthritis over time.
How tears occur:
Traumatic injuries - usually in younger, active people, from twisting on a bent knee (e.g., during football, soccer, netball, skiing). They often present with sudden sharp pain and swelling.
Degenerative tears - more common in older adults, due to gradual weakening of the meniscus tissue. These tears can occur with minimal trauma and frequently coexist with early arthritis.
Tears can be described by patterns such as radial, horizontal, bucket-handle, root, oblique, or complex tears. Some tears (such as bucket-handle types) can be unstable, causing the knee to lock, and usually require urgent surgical attention.
What are the symptoms of a meniscus tear?
Knee pain: localised along the joint line, typically on the inside or outside of knee depending on which meniscus is torn. The pain may be sharp, especially during squatting or twisting activities.
Swelling: Typically, the knee develops swelling 24-48 hours after injury due to fluid build-up from the meniscus tear.
Reduced motion: difficulty fully straightening or bending the knee due to irritation or swelling
Clicking or catching: the torn fragment may get trapped during movement
Locking: in unstable tears, the knee may suddenly become “stuck” and unable to straighten
Giving way: occasional sense of knee instability
Diagnosing a Meniscus Tear
Clinical examination – assessment for swelling, tenderness, mobility, and provocation tests specific for meniscal tears
X-rays – to exclude fractures and detect arthritis that might influence treatment decisions
MRI scan – the gold standard imaging for meniscal injuries, showing not only the tear but also cartilage, ligaments, and overall joint health
Treatment Options
Non-Surgical Treatment
Not all tears need surgery—many can be treated with a structured non-operative approach, especially degenerative tears.
RICE principle: Rest, Ice, Compression, Elevation in the acute setting
Physiotherapy: Strengthening of quadriceps, hamstrings, and hip muscles to restore balance, stability, and motion
Medications: Simple analgesia and anti-inflammatories to reduce pain and swelling
Injections:
Corticosteroid injections to reduce inflammation in degenerative tears
Hyaluronic acid (“gel” or lubricant) injections in selected cases with early arthritis
Time and structured rehab: Many stable meniscal tears improve over 6–12 weeks without surgery
In degenerative meniscal tears with underlying arthritis, surgery usually has little long-term benefit and conservative care is preferred.
Surgical Treatment
When symptoms persist despite conservative management, or the tear is unstable, arthroscopic (keyhole) surgery may be offered.
1. Arthroscopic Partial Meniscectomy (Debridement)
Removal or trimming of the damaged part of the meniscus
Best for irreparable tears or degenerative tears causing mechanical symptoms
Provides rapid symptom relief, but reduces the shock-absorbing capacity of the meniscus, increasing the longer-term risk of arthritis
2. Meniscal Repair
Re-joining the torn meniscus using sutures or fixation devices
More successful in younger patients, acute injuries, and tears in the vascular (outer) zone where blood supply aids healing
Often performed arthroscopically in an “all-inside” fashion, but sometimes requires an additional small open incision
Healing rates: 80–95% in selected cases
Preserves meniscus function, greatly reducing the risk of arthritis compared with debridement
3. Meniscal Root Repair
A root tear is when the meniscus detaches from its bony anchor on the tibia
Functionally, this is equivalent to losing the entire meniscus, leading to rapid joint damage if left untreated
Repair involves passing sutures through the root and securing them via bone tunnels in the tibia with a suture button
Essential for preserving joint health and preventing early arthritis
What to Expect From Surgery
Diagnostic arthroscopy is first performed to assess the entire knee—including cartilage, ligaments, and both menisci. The appropriate treatment (debridement vs repair) is then carried out.
Debridement: Faster recovery, typically returning to normal activities within 4–6 weeks
Repair: Longer rehab (3–6 months) to protect the repair, often delaying impact sports until healing is secure
Root Repair: Rehabilitation is more cautious, often non-weight-bearing on crutches initially, as the fixation heals into bone
Rehabilitation & Recovery Timeline
Key Rehabilitation Principles
Physiotherapy supervision is essential – exercises are tailored for strength, flexibility, and proprioception (joint awareness).
Early motion is encouraged to prevent stiffness, but loading is restricted for repairs in the healing period.
Return to sport testing is performed before full clearance, ensuring balance, power, and movement control are restored.
Reinjury prevention programs (agility, cutting, pivoting drills) reduce the risk of further tears.
Recovery after a meniscus tear depends on the type of treatment you receive. Preserving and repairing the meniscus often requires a slower rehab program than trimming it, but it provides far better long-term joint health.
Your recovery depending on what type of treatment you receive:
Non-Surgical (Physiotherapy, Injections, Rehab)
Weight Bearing: Immediate weight-bearing as tolerated
Return to Daily Activities: 2–6 weeks most patients walk normally with improved strength and stability
Sport/Running Timeline: Low-impact sports: 8–12 weeks; pivoting sports only if symptoms settle (often not recommended if arthritis present)
Key Notes: Best for stable or degenerative tears; focus is on strengthening and symptom control rather than “healing” the tear.
Arthroscopic Debridement (Partial Meniscectomy)
Weight Bearing: Full weight-bearing immediately post-surgery
Return to Daily Activities: Return to desk work within 1–2 weeks; more physical work 3–4 weeks
Sport/Running Timeline: Jogging usually at 4–6 weeks; full return to sport by 6–8 weeks
Key Notes: Quickest recovery but loss of shock absorption does increase risk of arthritis later.
Meniscal Repair
Weight Bearing: Often partial or non-weight bearing for the first 2–4 weeks (crutches used)
Return to Daily Activities: Desk work 2–3 weeks; more physical jobs 6–8 weeks
Sport/Running Timeline: Running begins around 3–4 months; pivoting/impact sports delayed to 6–9 months
Key Notes: Preferred if repairable – preserves meniscus, lowers risk of arthritis. Rehab is deliberately slower to protect the healing repair.
Meniscus Root Repair
Weight Bearing: Non-weight bearing 4–6 weeks (crutches required) to protect fixation
Return to Daily Activities: Everyday walking 8–12 weeks with support, depending on progress
Sport/Running Timeline: Running 5–6 months; pivoting/contact sports often delayed 9–12 months
Key Notes: Root tears are high-risk for arthritis if untreated. Repair has excellent long-term outcomes but requires patience with longer initial restrictions.
What are the risks of meniscus surgery?
Infection, bleeding, or damage to surrounding structures (rare)
Persistent pain or stiffness
Meniscus re-tear
Meniscectomy increases the long-term risk of arthritis
Meniscal repair may fail if the tear is in an avascular (non-healing) zone or if rehab protocols are not followed
What is the prognosis?
Debridement: Provides rapid short-term relief, particularly for mechanical symptoms, but can accelerate joint degeneration
Repair: Preserves meniscus function, has excellent healing potential in appropriate cases, and reduces arthritis risk long-term
What about meniscal cysts?
Meniscal cysts form when joint fluid escapes through a tear, creating a cyst beside the meniscus (usually on the outer side of the knee)
Presents as a painful lump in young to middle-aged adults, commonly on the outside of the knee
Treatment involves addressing the underlying meniscus tear (repair or debridement), along with drainage or excision of the cyst. Occasionally in large cysts an open incision is required.