Revision Hip Replacement
Revision hip replacement is a complex but highly effective operation designed to give patients a second chance at a stable, pain-free hip when their initial replacement has failed. With careful planning, modern implants, and structured rehabilitation, most patients regain excellent function and independence.
What is a revision hip replacement?
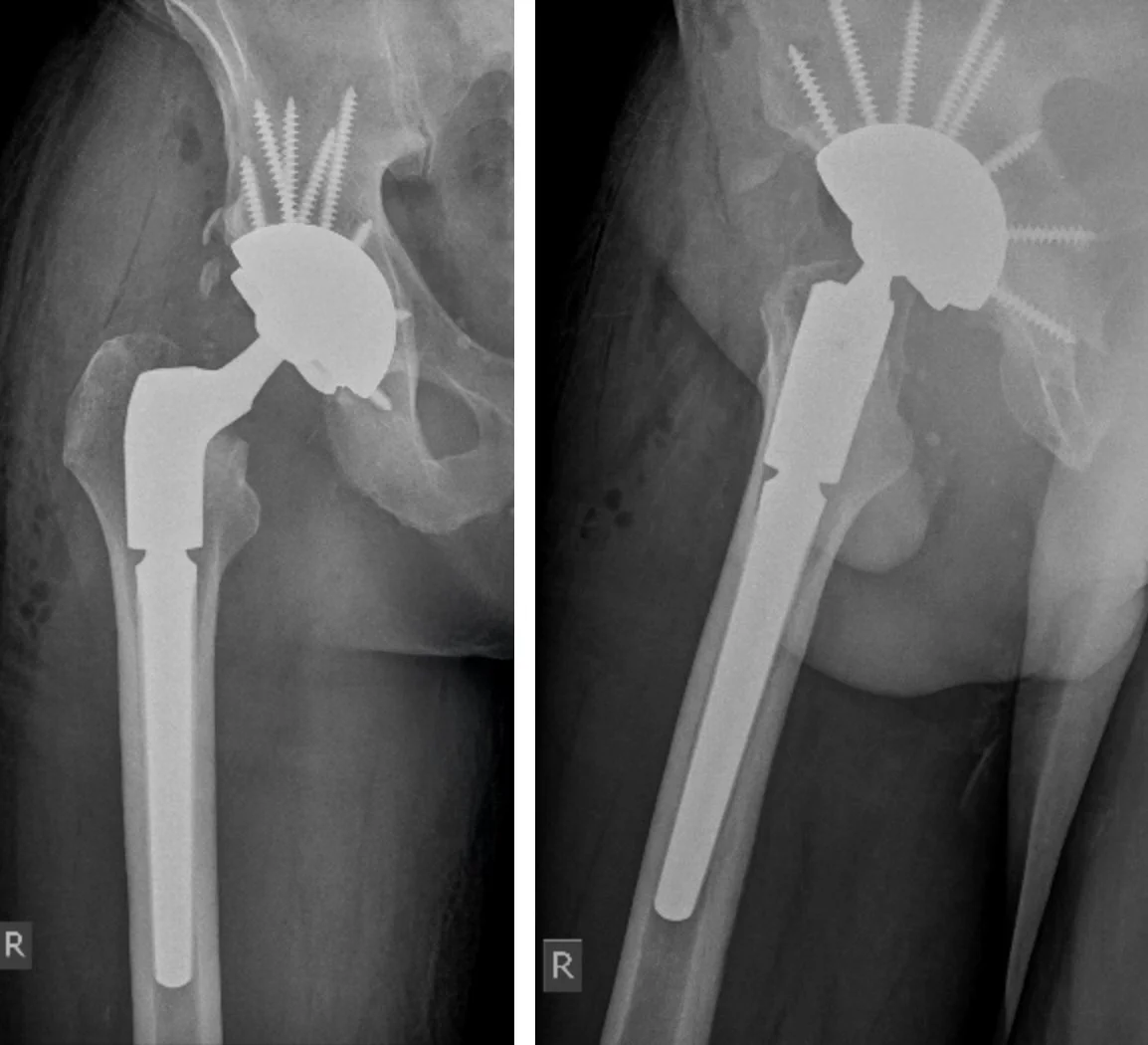
A revision hip replacement is an operation performed when your original hip replacement no longer works properly. This may involve removing some or all of the old implants and replacing them with new components. Unlike a first-time (primary) hip replacement, revision surgery is often more complex. This is because there may be scar tissue, damaged bone, or infection that needs to be carefully managed. In some cases, bone grafts or special implants are used to rebuild and stabilise the hip.
The main goals are to:
Relieve pain
Restore a stable and well-functioning hip
Correct leg length and alignment
Allow you to return to everyday activities with confidence
Indications for Revision Hip Replacement
Revision hip surgery may be recommended for:
Implant wear or loosening
Infection of the prosthetic joint
Instability or recurrent dislocation
Persistent pain or stiffness
Fracture near the prosthesis (periprosthetic fracture)
Bone loss around the implant (osteolysis)
Mechanical failure or fracture of the implant components
Preoperative Assessment
A thorough assessment is crucial before revision hip replacement. This helps identify why the first replacement failed and ensures the surgery is carefully planned.
The workup usually includes:
Clinical assessment: A discussion of your pain, mobility issues, or instability, as well as a physical examination.
Imaging: X-rays, CT, MRI, or a CT SPECT scan may be used to assess implant position, fixation, bone stock, and any fractures or loosening.
Blood tests and joint aspiration: Used to check for infection; joint fluid is sometimes collected and analysed for bacteria.
Medical and surgical history review: Including your original surgery details, implant type, other medical conditions, and anaesthetic considerations.
This preparation ensures the revision surgery is appropriately indicated and performed as safely as possible.
What is involved in a Revision Hip Replacement?
The revision procedure generally includes:
1. Surgical approach
The hip is usually accessed through your previous incision. In some situations, another approach may be chosen for better access or safer surgery.
2. Removal of old implants
The worn or loose components are carefully removed. Any previous cement is also taken out. In cases where implants are very secure, bone cuts (osteotomy) may be necessary to safely remove them.
3. Reconstruction of bone and soft tissues
If bone has been lost, it may be rebuilt with bone grafts, metal augments, or specialised implants. Soft tissues around the hip are balanced to restore stability.
4. Insertion of new components
Stronger and often larger revision implants are used. These may be secured with screws, bone grafts, or other fixation methods for added stability.
5. Closure and recovery
The incision is closed, sometimes with a drain to reduce swelling. Rehabilitation begins early, guided by your physiotherapist.
Recovery After Revision Hip Replacement
Recovery tends to be slower than with a first-time hip replacement, because the surgery is more complex. However, with proper rehabilitation, most patients regain excellent function and pain relief.
Typical follow-up schedule:
2 weeks: Wound check and dressing removal. Results from tissue samples are reviewed.
6 weeks: Clinic review and X-ray. By now most patients can walk without a stick or crutch.
3 months: Further X-rays are taken. Patients are usually walking longer distances and find daily activities much easier.
12 months: By this stage, most patients are pain-free with good function. An X-ray checks for implant stability.
Long-term: Follow-up every 5 years with repeat X-rays to check implants remain stable.
Special Case: Two-Stage Revision for Infection
When infection is present, a two-stage revision is often the safest and most effective approach. It is considered the gold standard in treating chronic prosthetic hip infections.
First Stage: Removal and Infection Control
Removal of the old prosthesis and infected tissue.
Thorough cleaning (debridement) of the joint.
Placement of an antibiotic-impregnated spacer to maintain the joint cavity and deliver local antibiotics.
Intravenous and oral antibiotics for 6–8 weeks, adjusted for the specific bacteria.
Interim Period
Follow-up with blood tests, scans, and sometimes repeat aspirations to confirm infection is cleared.
Second Stage: Re-Implantation
Removal of the temporary spacer.
Reconstruction of the hip with new implants, which may be larger or reinforced with screws, augments, or bone grafts.
Start of physiotherapy to restore hip movement and strength.
This process gives the best chance to clear infection and restore long-term hip function.
Frequently Asked Questions
What are the risks of revision hip replacement surgery?
Revision hip replacement carries a slightly higher risk profile than first time surgery:
Hip replacement surgery is generally safe but, like any major procedure, it carries risks. These include:
Blood clots: in the leg veins, which can travel to the lungs (pulmonary embolism). This risk can be reduced by early movement, blood thinners, and compression devices.
Infection: which is minimized by sterile surgical techniques and antibiotics. If you are concerned about an infection, please call the rooms and do not start antibiotics until speaking with Mr. Kirzner
Dislocation: more common than after primary hip surgery, but reduced with careful implant positioning and modern implant designs.
Leg length discrepancy: Many in the community have a small leg length discrepancy and aren’t even aware of it. After a hip replacement you will often feel longer than before surgery as your body has become accustomed to a short leg from arthritis. This feeling often settles with time. True leg length discrepancy is minimised with careful intraoperative planning. Lengthening or shortening the leg slightly may be apart of the surgical plan to improve your outcome.
Implant problems: loosening, wear, or rarely, mechanical failure may occur over time, sometimes requiring revision surgery. Most implants last over 20 years nowadays.
Nerve or blood vessel injury: though this is uncommon, nerve or blood vessels around the hip can be injured during surgery. Thigh numbness to the lateral thigh is relatively common with a direct anterior approach incision, this is due to damage/injury to the superficial nerve supplying the skin (lateral femoral cutaneous nerve).
Dissatisfaction or ongoing pain: : Rarely patients report ongoing pain and lack of satisfaction, often due to other sources of referred pain (lumbar spine, sacroilliac joint or other), tendinopathic conditions and/or muscle weakness. Every effort is made to avoid this with correct diagnosis, prehabilitation, and extensive discussions.
We will go through your personal risk profile and ensure that every step is taken to minimise complications and maximise success. The fitter and stronger you are prior to your surgery, the safer and quicker your recovery will be and the more you will get out of your knee. We take every precaution to reduce these risks and provide long-term success.
What Is a Two-Stage Revision?
A two-stage revision hip replacement is performed when an artificial hip joint becomes infected or severely damaged. It is considered the gold standard for managing chronic periprosthetic joint infections, as it offers the best chance to eliminate infection before replacing the failed implant.
First Stage: Removal and Infection Control
The infected prosthesis is surgically removed along with any inflamed or infected tissue (aggressive debridement).
The joint is thoroughly irrigated and cleaned to eliminate bacteria and necrotic tissue.
An antibiotic-impregnated spacer is placed in the joint to maintain alignment and deliver high local concentrations of antibiotics.
Systemic antibiotics are administered, typically for 6-8 weeks, tailored to the specific organism identified during surgery.
Interim Period
The patient receives continued medical treatment and monitoring to ensure complete infection clearance, often confirmed by blood tests, imaging, and possible re-aspiration.
Second Stage: Re-Implantation
Once infection has resolved, demonstrated by negative tests and healthy wound healing, the temporary spacer is removed.
The hip joint is reconstructed with new prosthetic components, designed for stability and function, usually requiring longer and bigger implants with additional screw fixation, augmentation or bone grafting if there has been bone loss.
The wound is closed, and the patient begins rehabilitation to regain strength and mobility.
Two-stage revision provides high infection cure rates but requires careful planning and a multidisciplinary approach due to its complexity and prolonged treatment period.
Outcomes: How Successful Is It?
While results are not always identical to those of a first-time hip replacement, most patients undergoing revision achieve:
Significant pain relief
Greater hip stability and confidence with movement
Improved quality of life and return to daily activities
Modern implants and surgical techniques mean that many revision hip replacements now last for 15–20 years or more.