Hip Osteoarthritis (OA)
What is Hip Osteoarthritis?
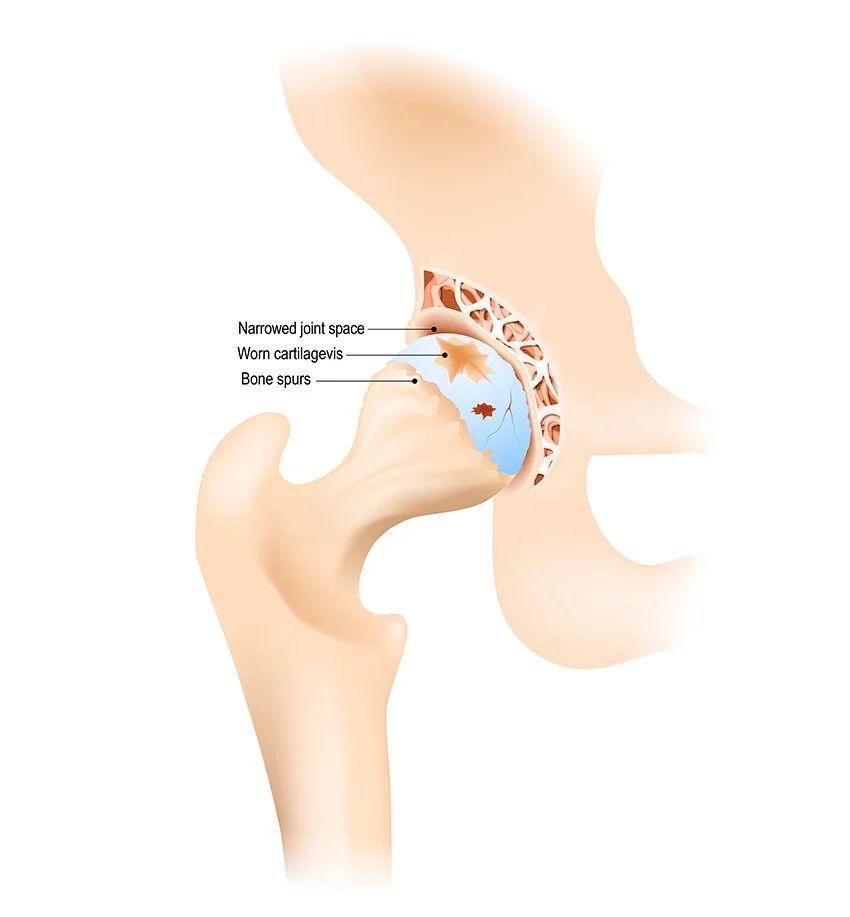
Hip osteoarthritis is a common condition where the cartilage that lines the hip joint gradually wears away. The hip is a ball-and-socket joint—the ball at the top of the thigh bone (femur) fits securely into the socket in the pelvis (acetabulum). This design allows for smooth, fluid movement in multiple directions while supporting the weight of your body.
A healthy hip joint has a thick layer of smooth cartilage covering both the ball and the socket. This cartilage cushions the bones, absorbs shock, and prevents painful friction. In osteoarthritis, the cartilage becomes thin, rough, or worn away. As a result, the ball and socket begin to grind directly against one another. Over time, this leads to pain, stiffness, inflammation, and difficulty with mobility.
What causes Hip Osteoarthritis?
There is often no single cause for hip osteoarthritis, but several factors contribute to its development:
Aging: Cartilage naturally degenerates with age, losing its ability to heal and repair itself. Hip osteoarthritis is increasingly common after the age of 50.
Previous injuries: Hip fractures, dislocations, or repetitive strain from sports and heavy physical work can accelerate wear and tear.
Hip shape and alignment: Some people are born with structural differences, such as hip dysplasia or impingement, that place uneven stress on the joint. This can cause earlier cartilage breakdown.
Family history: Genetics can predispose certain individuals to osteoarthritis at a younger age.
Excess body weight: Additional weight places greater pressure on the hip joint with every step, accelerating damage over time.
Symptoms of Hip Osteoarthritis
Osteoarthritis of the hip develops gradually, and symptoms may progress over several years. Common signs include:
Groin pain – usually the most common symptom, which may also radiate to the thigh, buttock, or even the knee
Stiffness in the hip, especially after rest or first thing in the morning
Pain that flares with activity such as walking, climbing stairs, or standing for long periods
Difficulty with everyday movements such as bending to tie shoes, getting in and out of a chair, or getting into a car
Limping or changes in walking pattern due to discomfort or restricted movement
Loss of hip motion over time, with difficulty rotating the leg or spreading the thighs apart
Night pain or disturbed sleep in more advanced cases
Treatment for Hip Osteoarthritis
Treatment is tailored to each individual, depending on the severity of symptoms, lifestyle, and goals. Non-surgical options are usually tried first, but surgery may be recommended if pain and disability progress.
Non-surgical treatments include:
Lifestyle and activity modification:
Managing weight to reduce load on the hip
Choosing low-impact activities such as swimming, cycling, and walking to stay active without worsening joint stress
Physiotherapy and exercise programs:
The GLA:D program (Good Life with Osteoarthritis in Denmark) is an internationally recognised education and exercise program shown to improve mobility and reduce pain in people with hip osteoarthritis. It focuses on targeted strengthening, functional training, and empowering patients to manage their condition.
Tailored physiotherapy exercises can improve hip flexibility, strength, and stability.
Medications:
Pain relievers (analgesics): Paracetamol or acetaminophen may help mild pain.
Anti-inflammatory medications (NSAIDs): Such as ibuprofen, naproxen or prescribed options like meloxicam, reduce both pain and inflammation in the joint.
Topical anti-inflammatory gels/creams: Applied directly over the hip area to help with pain relief.
Stronger pain relief: In select cases, short courses of prescription drugs such as tramadol may be used, but these are generally not a long-term solution.
Joint and injection therapies:
Corticosteroid injections: Can provide short-term relief of inflammation and pain.
Viscosupplementation (hyaluronic acid injections): Though less commonly used in hips than knees, in some cases may provide lubrication and symptom relief.
Emerging therapies (PRP, stem cells): Research is ongoing; these are not yet standard but may be considered in select individuals.
Supportive aids:
The use of a walking stick, cane, or crutches can offload weight and reduce pain.
Shoes with cushioned soles or inserts may improve joint protection.
Surgical treatments include:
Hip arthroscopy: A minimally invasive “keyhole” procedure to correct structural problems, usually in younger patients with early osteoarthritis.
Osteotomy: Re-shaping the bones to relieve pressure on the damaged part of the joint, occasionally suggested for younger individuals.
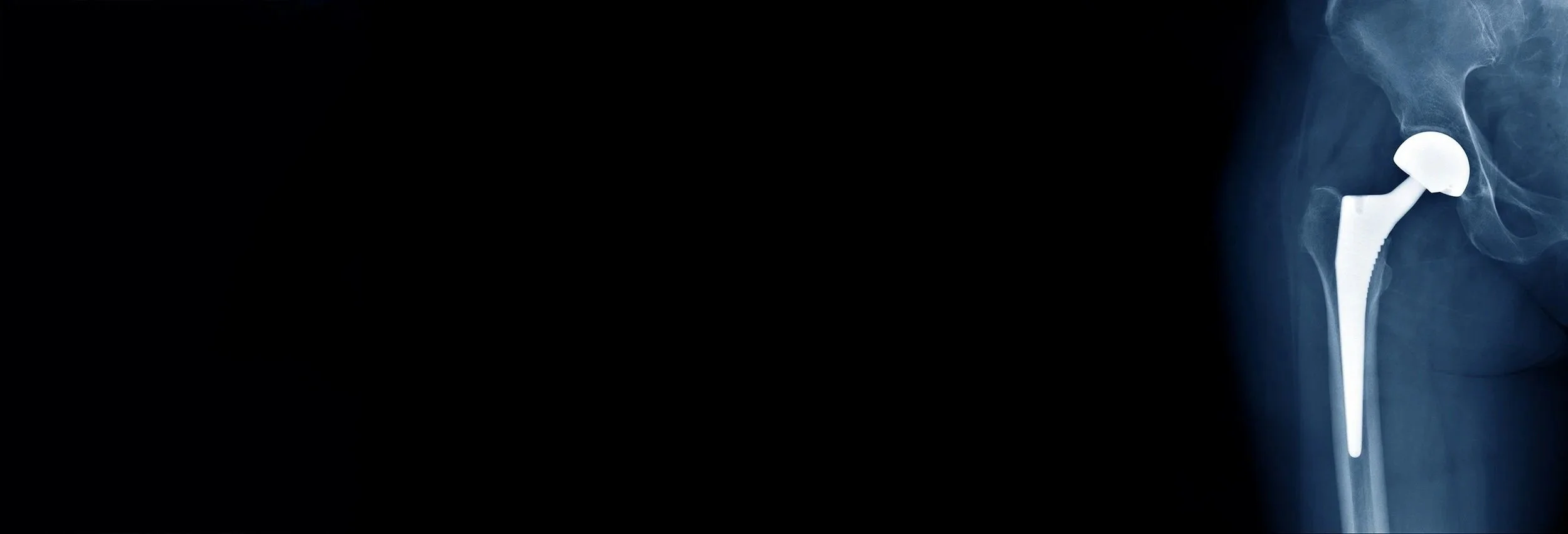
Total hip replacement: The most definitive treatment for advanced hip osteoarthritis. In this procedure, the worn joint surfaces of the ball and socket are replaced with smooth, durable artificial components. This operation is highly effective in restoring mobility and significantly improving quality of life.
When to see a Specialist
You should consider seeing Mr. Kirzner if:
You experience persistent pain in the hip or groin area that limits your daily activities
You find it difficult to walk, climb stairs, or bend over
Hip stiffness makes it hard to move or rotate your leg
Pain interferes with your sleep or quality of life
Symptoms are not improving despite non-surgical measures
During a consultation, Mr. Kirzner will assess your hip with a thorough examination and imaging if required. Together, you can explore the most appropriate treatment options for your stage of osteoarthritis and personal goals. The focus is on relieving pain, improving your mobility, and helping you return to the activities that matter most to you.